
Background
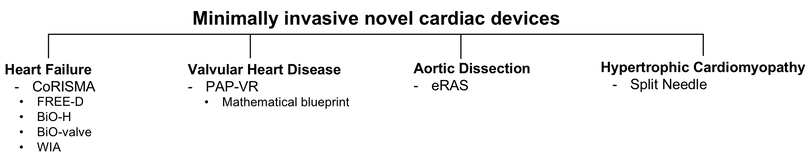
One in every four deaths in the U.S. is related to heart disease, killing more people every year compared to all cancer deaths taken together. Open-heart surgeries are often used to treat patients with heart disease which requires very restrictive patient selection criteria due to its invasiveness. As life expediencies rise and older population grows dramatically, reducing the invasiveness of surgical therapy is becoming increasingly vital. A transcatheter cardiac assist device combined with a wireless power transfer system can be a fundamental solution to reduce the invasiveness of the current cardiac devices. The following diagram summarizes product lines I have been working on since I joined Yale Artificial Heart Lab in 2017, which culminated in founding the startup company Bonde Innovations LLC in 2018.
Transcatheter technique


Heart failure
Left ventricular assist device (LVAD) therapy has changed the natural history of end-stage heart failure patients. Heart failure is the leading cause of death affecting more than 6.5 million Americans. Transplant is a limited resource available only for 3,000 patients every year. Randomized trials have shown a 50% survival benefit with LVAD (left ventricular assist device) when compared to medical management who cannot get a transplant. However, LVAD therapy is still hampered by several adverse events related to the following issues. We came up with a new concept of artificial heart pump called CoRISMA, Co-Rhythmic, Isolable, Self-Maintenance, Assist, which tackle all these issues.


CoRISMA prototypes

Long-range configuration



-
Wireless power transfer system
One distinct difference between any implantable medical device such as pacemakers, artificial knee or hips, and LVAD is the presence of a permanent electrical cable that penetrates the abdominal wall to connect to a controller and batteries. Besides acting as a constant nidus for infection, this also leads to overall less acceptance by patients, poor quality and leads to a cumbersome tethered existence. The FREE-D system uses magnetically coupled resonators to seamlessly supply energy to an LVAD, without compromising mobility or requiring direct contact between the patient and the energy source as in the previous transcutaneous energy transfer system (TETS) applications.
-
In-vivo VAD maintenance
The ventricular assist device (VAD) requires 24 hours a day/7 days a week/365 days a year (24/7/365) continuous operation. However, there has been no technological innovation that allows this pump to be serviced. This is akin to driving a car without changing its oil and filter or doing any maintenance for five to ten years. In current VADs, there is no access to clean the pump without highly invasive open-heart surgery. The in-vivo VAD maintenance system incorporates a unique component called Balloon isolation Occluding valve (BiO-valve) which isolates the pump from the circulatory system and allows local access to the pump. A major strength of this system is that all four steps of the procedure, isolation, purging, maintenance, and service are accomplished while VAD is implanted inside the body. The pump can last longer if it is constantly cleaned/maintained and serviced as is the norm in the pump industry.


-
Novel impeller design
A fundamental footprint of an impeller design in an artificial heart pump has remained unchanged since the first design of rotary VAD in the 1980s. New impeller designs that have completely different footprint from conventional Archimedean screw-based impeller designs may provide important new insights on artificial heart pump designs and operations. A key characteristic of this conventional impeller design whether axial or centrifugal is a limited space that is available within the rapidly alternating blades attached along a central hub which forces blood cells to pass over. I have presented a rotary displacement pump with taegeuk pattern of impeller incorporated to create pulsed operation without using pneumatic actuation. I have also designed and demonstrated a hemodynamically superior impeller, called Biologically inspired, Open, Helicoid (BiO-H), inspired by an avian right atrioventricular valve30. The BiO-H shows an improved flow path with 2.25-fold less area loss than the conventional impeller designs.
-
Heart monitoring by wave intensity analysis (WIA)

The current assessment of ventricular dysfunction is based solely on pressure and echocardiographic assessments, which are both operator dependent and variable. Thus, the ventricular assessment remains primitive and difficult to assess dynamically over the course of patient care. The main focus of the study was to quantify the wave energy in either ascending aorta or the main pulmonary artery that is produced by a dysfunctional left (LV) or right ventricle (RV) respectively. The LV&RV wave patterns were quantified over a range of physiologic conditions, for example with different operation modes (continuous vs pulsed) and different physiological interventions (increased afterload vs preload), for both centrifugal and axial pumps. The physiologic controller combined with WIA can provide a robust and quantitative metrics of LV&RV dysfunction, an objective criterion to diagnose the onset of LV or RV failure.

Valvular Heart disease
About 4.1 million people suffer from moderate to severe mitral regurgitation (MR, a leak from the mitral valve) in the U.S. and 30% (1.67 million) of this population is eligible for treatment. However, only 2% (30k) of this population is considered operable candidates, the rest is considered too sick since the ventricle is considered too dilated with significant separation of papillary muscles that leaflet approximation alone would not reduce the leak from the valve. With 3D mathematical modeling and simulation of mitral valve dynamics, I have shown manipulating papillary muscle position can be a fundamental solution for these inoperable patients. Papillary muscle approximation is a verified subvalvular remodeling surgical technique but requires open-heart surgery with time-consuming and technically demanding procedures involved, which is not applicable for high-risk surgical patients. The PAP-VR (Papillary Muscle Approximation & Ventricular Restoration) system is a novel transcatheter mitral valve repair system that will address the root cause of the majority of MR and expand the patient pool.

Aortic Dissection
Type A dissection repair requires highly invasive surgery with circulatory arrest, mortality and morbidity following surgery remain high and poor-risk patients are often not considered surgical candidates. Endovascular repair of Type A dissection is hampered due to problems with fixation, migration, and obliteration of the false lumen. The eRAS (Endovascular Reconstitution of Aortic Sinotubular Junction for Type A Dissection) is an anatomically inspired system, a reproducible and novel magnetized stent construct which tackles all these issues with ease and reliability.

Hypertrophic Cardiomyopathy
Surgical myectomy is highly invasive and sometimes a residual gradient means doing a re-do sternotomy with added morbidity and mortality. A transcatheter septal myectomy can greatly improve the management of the patients with the ability to perform customized myectomy with simultaneous measurement of gradient and hemodynamics. And an ability for re-invention at little risk of comorbidity. The Split Needle has a core capture, the innermost part of the device, which incorporates suction cup arrays to vacuum a portion of tissue toward the aperture. Once the core is captured cutting edge transect the core which is then transported out through the catheter. Series of cores can be sliced on demand to yield a gram of cylindrical tissue core for each pass.
